Vagus Nerve Stimulation (VNS) therapy is a form of treatment for people whose seizures are not controlled with medication alone. VNS Therapy aims to reduce the number, length, and severity of seizures.
Response to VNS therapy can vary from person to person and happens over a period of time. The response to VNS may not be noticed for up to a year. Other benefits reported are improved mood, memory, and alertness. VNS is used alongside anti-seizure medication.
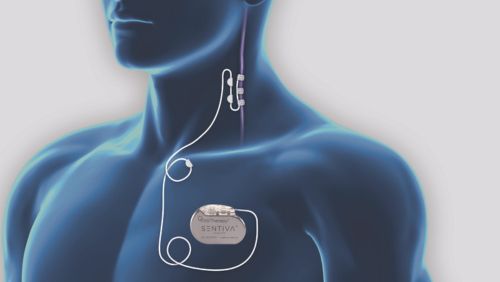
The VNS device is similar to a cardiac pacemaker, and it is battery-powered. The VNS device/generator is inserted under the skin of the chest wall on the left side, with a wire attached to the left vagus nerve. The VNS device sends regular, mild electrical stimulation to the brain via the vagus nerve which in some people with epilepsy reduces the frequency and intensity of seizures. The VNS pack also includes a magnet for manually helping to control your seizures by giving extra stimulation. This will be explained to you if you are suitable for VNS therapy.
The Model M1000 or ‘SenTiva’ is the device currently being used. This device has an auto stimulation which detects when the heart rate increases and uses that as an indication that the person is having a seizure. When activated, it gives off stimulation to help abort the seizure. It also has the ability to be programmed to increase at small intervals if you are having it implanted for the first time, so you don’t have to return to the hospital as frequently. It helps you reach a target level quicker.
The battery life of a VNS generator depends on the settings. However on average it can last for 3-5 years, before being replaced. You will require an operation to replace the VNS battery once it has run out, this usually takes around 45 minutes.
Having a new VNS inserted

You are admitted to hospital for insertion of a new VNS. You will usually stay for 2 nights. You will have a general anaesthetic to have your VNS inserted in theatre; the operation usually takes about 2 hours. You will have 2 incisions, one on your neck and one on the left side of your chest.
You will be reviewed again by your neurosurgical team the morning after your operation and discharged home with a prescription for pain relief. The Epilepsy Surgery Nurse will meet with you before you leave and give you information on how to care for your VNS wounds, and when to have your stitches removed. There is a small risk of infection at the incision site.
An appointment will be arranged for you to attend your referring Neurologist or VNS clinic for switch on and education of your new VNS device, two-four weeks after your operation.
After the operation
You will continue to take your Anti-seizure medication as prescribed by your Doctor. You will follow up with your neurology team who will manage your VNS settings. You will have regular appointments to adjust and manage your VNS settings to a tolerable level where it is hoped the treatment may stop, shorten or reduce the severity of your seizures. Each person's response is unique.
The below list outlines key information to be aware of post-insertion of a VNS device:
- Possible Side Effects: VNS therapy may cause side effects during the time that the nerve is being stimulated. Side effects usually reduce over time or with adjustments to your VNS setting. Some common side effects are – hoarseness, coughing on stimulation.
- No Response to VNS therapy: It is rare to not have any response to your VNS, but if this is the case, your Neurologist may consider having the device switched off. If you choose to have your VNS removed, the leads are usually left in place; this may cause problems if you need MRI imaging at a later stage. It is usually recommended to leave the device in place, switched off. If VNS therapy has no effect on your seizures, it may have other positive effects, such as improved mood, alertness and wellbeing.
- MRI scan and VNS therapy: If you have a VNS device and need an MRI, you must have your VNS switched off before the scan and switched back on afterwards. You can arrange this with your Neurology team. Certain MRI scanners are not suitable for patients with VNS; your Neurology team will advise you about this. CT scans and X-Rays do not affect VNS therapy.
- VNS Battery Replacements: If you are benefiting from VNS therapy, your Doctor will recommend that you have the battery replaced when it starts to wear down. This will be noticed by your neurology team when they check your VNS at your appointments or you may notice an increase in your seizure frequency. The team will refer you for a VNS battery replacement, this operation usually takes about 45 minutes. You will be admitted to hospital for one or two nights, you will be put to sleep to replace the VNS battery in theatre. Usually the original neck leads remain in place. The Neurosurgeon will reopen then chest scar from your VNS, remove the old VNS and place a new generator (VNS) into the same site. Your VNS will be switched on the following day by the Epilepsy Surgery Nurse, who will also give your discharge information on wound care and arrange for you to follow up with your usual neurology team. You will attend your GP to have your chest stitches removed 12/14 days after the operation.
You can find further information on VNS therapy by visiting the 'LivaNova' website. LivaNova are the company that manufacturer the VNS device.
